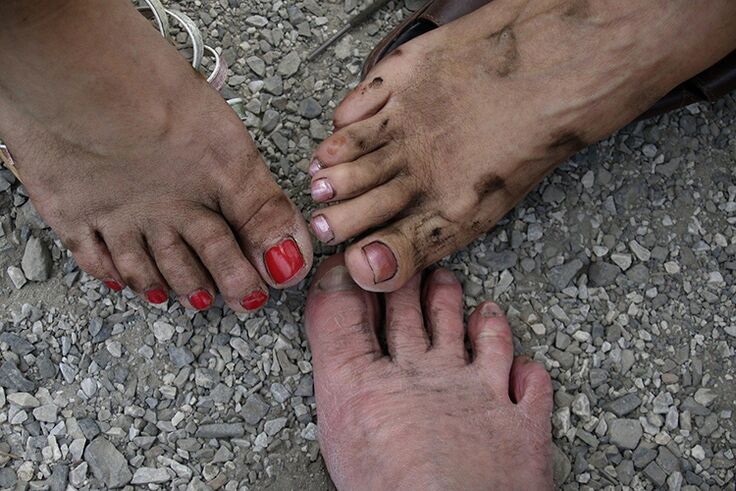
Mycoses of the skin are a common group of diseases. Patients do not always take them seriously enough, leading to advanced forms of pathology that are difficult to treat. Fortunately, there are many ways to get rid of a fungal infection on your feet and get rid of a nasty disease such as a fungal infection of your toes and feet.
Patients do not always take them seriously enough, leading to advanced forms of pathology that are difficult to treat. Fortunately, there are many ways to get rid of a fungal infection on your feet and get rid of a nasty disease such as a fungal infection of your toes and feet.
Skin mycosis between the fingers - how does the disease occur?
Skin mycosis is an infectious disease caused by fungi that parasitize the skin. They can appear anywhere on the body. But more often they choose skin folds. The places between the toes are their favorite places. This is due to the fact that the feet often sweat and in tight shoes the moisture does not have time to evaporate. Therefore, the areas between the fingers are often wet and damp. And it is under these conditions that the fungus is needed for reproduction. It is not uncommon for the fungus to penetrate the recesses between the fingers from the infected nails.
Contribution to the development of skin disease:
- inadequate foot hygiene, overheating or hypothermia;
- tendency to increased sweating;
- poor blood circulation in the foot associated with heart disease, smoking, diabetes mellitus;
- tension;
- calluses and cuts on the skin of the foot;
- lack of vitamins and minerals (mainly zinc) in the body;
- trophic ulcers on the foot;
- hormonal imbalance and thyroid disease;
- overweight;
- excessively dry skin.
However, in most cases, a fungus between the toes does not develop if a person has healthy immunity.
The disease is more common in men due to more frequent wearing of tight shoes. The fungus can appear on the feet not only in adults but also in children.
Skin mycosis between the toes in 90% of cases is caused by three types of fungal activity from the group of dermatomycetes - Trichophyton, Microsporum, Epidermophyton. In addition, the skin of interdigital spaces is often affected by fungi of the genus Candida.
Most often, the infection initially develops in the cavity between the two smallest toes. However, other interdigital spaces may also be affected. Once in the skin, the fungus actively multiplies on it. The remnants of the stratum corneum of the skin serve as food for microorganisms.
The skin infection can spread from person to person. For this, simple contact of the skin of the foot with the surfaces containing the fungus is sufficient. The spread of the pathogen can be done with the help of other shoes, socks, shared towels and a wet floor in the shower. Personal hygiene should be carefully monitored, use only personal items. In the swimming pools, use showers, baths and saunas with personal or disposable slippers and slippers.
It often happens that a skin condition spreads from one family member to another, with the same shoes, pedicure, socks, towels, barefoot walking, and so on.
Symptoms of a fungal infection on the skin of the foot.
Symptoms of leg mycosis in the early stages:
- itching and burning, worse at night;
- drought;
- exfoliation of the skin;
- small cracks.
As the disease develops, the symptoms intensify, the itching and burning become unbearable, leading to scratches and skin irritation, and the cracks deepening. The skin of the foot becomes rough. Pain appears, unpleasant odor that does not go away even after washing, edema and hyperemia, the epidermis comes off.
Bubbles filled with serous fluid then appear. Once opened, non-healing, peeling ulcers remain on the skin. Bacterial is associated with mycotic infection.
Exfoliation of nails, abscesses may appear. A complication of mycosis of the foot can be the penetration of the fungus into the bloodstream and the spread of the infection throughout the body. At the same time, body temperature rises. Gangrene lesions of the foot can also develop. Cardiovascular diseases, immunodeficiency conditions, and diabetes mellitus complicate the course of skin disease.
To diagnose foot mycosis, it may not be enough for your doctor to examine your skin. It is often necessary to analyze the composition of the skin microflora. To do this, they get a scratch from the affected surface. The fungus can be found on the skin even if there are no visible symptoms of infection.
There is also a popular method for determining the presence of a fungus on the foot. To do this, place your feet in a potassium permanganate bath. If there are no fungi on the skin, it will turn pink and the affected areas will be white.
How to remove fungus between the toes?
It is very easy to get an infection on your skin, but it is much harder to get rid of it. Mycoses of the skin are always treated at home, but this does not mean that the patient is definitely helped by a completely independent treatment. In any case, a doctor's consultation is required.
There are a number of antifungal drugs that effectively kill fungi. However, the success of treatment depends largely on the stage of the disease. If you have gone too far, it will be difficult to get rid of the infection. In the initial stage, external antifungal drugs are used. If the disease is already running, doctors recommend treatment by systemic means. Terbinafine, itraconazole, fluconazole are most commonly prescribed in tablet form.
Popular antifungal agents:
- nystatin,
- fluconazole,
- ketoconazole,
- clotrimazole,
- terbinafine,
- naftifin,
- miconazole,
- itraconazole,
- natamycin.
Some antifungal ointments also contain anti-inflammatory ingredients.
All ointments are applied in the same way - they should be applied regularly in a thin layer to the affected areas of the skin. Some ointments are sufficient once a day, others require more frequent application. Antifungal sprays that can be sprayed on the affected area are even more convenient than ointments.
Treatment with antifungal ointments can be lengthy. Some types of ointments can get rid of the infection after 2 weeks. But in the case of severe damage, the duration of treatment can take up to 3 months. Doctors advise that the ointment be applied at least 2 weeks after the visible symptoms of the disease have passed. And once every six months, the toes should be lubricated with ointments for preventative purposes.
Systemic antifungal drugs may also be used in severe infections. However, they have a long list of contraindications and side effects. Especially anti-fungal tablets are contraindicated in pregnant women. In addition, many skin ointments are prohibited during pregnancy. If the use of such topical preparations is required, a doctor should be consulted. Not all medicines are allowed in childhood. Therefore, you should consult the instructions for the selected device. Some medicines can be used from the age of 2 years, others from the age of 12 years.
The specialist should select the appropriate medication. Improper use of antifungal drugs not only does not rid the patient of the pathogenic microorganisms, but can also lead to the development of resistance in them (especially in circumstances where the patient is continually re-infected). Toxins secreted by many fungi suppress local immunity, which further contributes to the development of infection.
In addition, vitamin and mineral complexes are taken up. If the disease is complicated by a bacterial infection, the doctor will prescribe antibiotics, but if there are allergic symptoms, they will prescribe antihistamines. The treatment can be supplemented with anti-inflammatory ointments, salicylic acid, sulfuric acid, ichthyol and zinc ointments.
Salicylic ointment:
- has antiseptic properties,
- prevents keratinization of the skin,
- promotes the repair of the epidermis,
- prevents the spread of infection.
Zinc ointment contains lanolin, menthol, zinc oxide. Zinc ointment has antiseptic properties, promotes skin regeneration, relieves itching and burns.
Sulfur ointment has anti-inflammatory, emollient and disinfectant properties. Ichthyol ointment is keratolytic, anti-inflammatory and bactericidal. In addition, ichthyol ointment promotes tissue regeneration.
Let’s not forget foot hygiene either. It is necessary to give up tight, uncomfortable shoes, synthetic socks and stockings, change the insole regularly. Shoes should be disinfected with an antimycotic spray. In fact, the treatment has no effect if the patient’s skin is constantly infected with new parts of the fungus that lives in the shoes.
Mushrooms between the toes: treatment with folk remedies at home
Treatment with pharmaceuticals does not always produce the desired effect. Therefore, people turn to folk remedies. This approach is also understandable because many synthetic antifungal ointments and sprays are not cheap at all. Treatment with folk remedies can be supplemented with treatment with pharmacy skin ointments.
The simplest folk remedies for getting rid of the fungus are salt and soda baths. To prepare the trays, you need 2-3 tablespoons of salt or baking soda per 5 liters. water. Water temperature - + 40-45 ° C The duration of the process is 15-20 minutes.

One of the best home remedies is an herbal bath with antiseptic properties. It can be chamomile, sage, marigold, nettle, St. John's wort. You need 2-3 tablespoons to make the bath. the herbal ingredients (you can use a mixture of different herbs) stick to a glass of boiling water, strain and add to a 5-liter pot of water for a bath. The water should be warm, but do not burn the skin of the feet. The duration of the procedure is 15-20 minutes.
Many people are also helped by baths with a solution of potassium permanganate on the skin of the feet in the presence of the fungus. Only a few grains of potassium permanganate are needed to make a light pink solution. You can also moisten the cotton pads with a potassium permanganate solution and insert it between your fingers.
Boric acid is also effective in treating the disease. You can also use liquid boric acid and powder. Acid can be added to baths and treated with affected areas.
You can also use a slightly warmed 9% apple cider vinegar solution for the trays. The duration of the procedure is 15 minutes. You can also make vinegar creams.
Another recipe is iodine baths. To prepare the solution, it is sufficient to dilute 20 drops in 3 liters of warm water. The duration of the procedure is 15 minutes, the course of treatment is 2-3 weeks.
After completing the aqueous procedures, the skin should be cleansed of keratinized and flaky tissues. It is recommended that baths be performed at least once a day, preferably at night.
In addition, you can use garlic ointment, pharmacy anti-dandruff shampoos with antifungal ingredients, creams with chlorhexidine and hydrogen peroxide to treat foot mycosis.
Prevention of skin mycoses of the toes
The disease is caused by non-compliance with the rules of personal hygiene. It is therefore necessary to:
- do not use pedicure tools, towels, slippers, socks and shoes of others, do not allow strangers to use their shoes, socks, hygiene equipment;
- maintain foot hygiene, wash skin daily with soap, carefully treating interdigital spaces;
- cut your nails regularly;
- wear comfortable shoes and socks made of breathable material;
- change socks regularly, wear socks washed at a temperature of at least + 40 ° С;
- exercise to improve blood circulation in the legs.
What is the fastest treatment?
It is impossible to say clearly which cure is the fastest and best. After all, the effectiveness of therapy for fungal diseases of the skin depends on many conditions - the severity of the pathology, the level of immunity, the presence of concomitant diseases. Some patients use traditional methods, others - pharmaceutical ointments help. It is important not to start the disease and start treatment with the first symptoms. It is also important to identify the type of pathogen. You should see a doctor for this. Maybe you will be able to find the best solution for your medicine.
























